BEAR® Implant

Dr. Gilmer is pioneering the use of a breakthrough technology called the BEAR® Implant for treatment of anterior cruciate ligament (ACL) tears, one of the most common knee injuries in the U.S.
The BEAR Implant is the first innovation in ACL tear treatment in more than 30 years. It is the first FDA-approved medical technology to enable healing of a torn ACL. This new approach is a shift from the current standard of care, reconstruction, which replaces the ACL with a graft.
Every year, approximately 400,000 ACL injuries occur in the U.S. A torn ACL does not heal without treatment, resulting in ACL reconstruction being one of the most common orthopedic procedures in the U.S. Yet the procedure has drawbacks; some procedures require two separate incisions, and some people who undergo reconstruction are unable to return to the same level of daily activities or sports.
There are a number of advantages to restoring a ligament instead of replacing it, and this exciting medical technology is the first to enable the body to heal its own torn ACL while maintaining the natural knee anatomy.
What does the procedure entail?
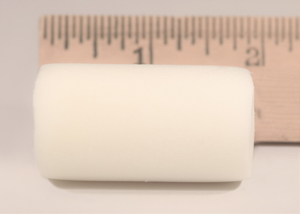
Unlike reconstruction, the BEAR Implant does not require a second surgical wound site to remove a healthy tendon from another part of the leg or using a deceased donor’s tendon. Instead, the implant acts as a bridge to help ends of the torn ACL heal together.
The surgeon injects a small amount of your own blood into the implant and inserts it between the torn ends of the ACL in a minimally invasive procedure. The combination of the BEAR Implant and your blood enables the body to heal the torn ends of the ACL back together while maintaining the ACL’s original attachments to the femur and tibia. As the ACL heals, the BEAR Implant is resorbed by the body, usually within eight weeks.
Who is the procedure for?
In general, the BEAR Implant is recommended for patients at least 14 years of age, skeletally mature (done or nearly done growing), with a complete rupture of the ACL, as confirmed by MRI. You must have an ACL stump attached to the tibia to facilitate the restoration. The BEAR device must be implanted within 50 days of injury.
Additional considerations are the related injuries, such as damage to cartilage, meniscus, or other ligaments, patient activity goals, and history of previous surgeries or injuries to the knee.
To determine if you are a candidate for the BEAR procedure, please see Dr. Gilmer’s remote consultation page: https://www.briangilmermd.com/remote-consultation-knee-sports-medicine-specialist-reno-nv/
What are the benefits?
About half of people who receive patellar tendon grafts experience pain while kneeling, and those who receive hamstring grafts have persistent weakness – as much as a 50% deficit at two years. Since the BEAR Implant doesn’t involve a graft, these types of complications don’t occur.
Additionally, both ACL reconstruction approaches have an ACL re-tear rate as high as 20% for teens and as high as 9% for adults. If the ACL is re-injured, revisions to traditional ACL reconstruction can be complicated and can require multiple surgeries. Conversely, revisions with the BEAR Implant are easier and more predictive.
Unlike reconstruction, the BEAR implant does not require a second surgical wound site to remove a healthy tendon from another part of the leg or use of a deceased donor’s tendon.
The BEAR Implant has the same potential medical/surgical complications as other orthopedic surgical procedures, including ACL reconstruction. These include the risk of re-tear, infection, knee pain, meniscus injury and limited range of motion. Each case carries unique risks and potential benefits. Dr. Gilmer can provide more information regarding the risks and benefits at an in person or virtual consultation.
If you’ve injured your anterior cruciate ligament, and may be interested in this technology, please see our recommendations for “Pre-habilitation” which can benefit almost anyone with an acute knee injury, https://www.briangilmermd.com/pdf/acl-prehab-gilmer.pdf and reach out via the Contact Us page by email or phone or by submitting a form directly through the website. https://www.briangilmermd.com/contact-us-knee-sports-medicine-specialist-reno-nv/
Dr. Gilmer’s approach
After reading the available medical literature and trialing carefully selected cases, I am excited about the potential that the BEAR implant may have for some patients.
I have conducted ACL repairs (sewing the patient’s own ligament back to the bone instead of replacing it) since 2015, but these have been in very selected cases. The reason is because the ACL has to tear in a very unique way for this to be successful. In studies dating back to the 1980s there was a high failure rate of ACL repair and that in part led to widespread adoption of reconstruction techniques. However, a smaller subset of these patients, skiers in particular had lower energy twisting injuries that tore the ligament from the bone but did not rip apart the fibers in doing so. Within that smaller population, again many of which were skiers, there were good long term results. This led me to look for these patients who might be good candidates for primary repair and with time we have been able to identify these better and classify patients better according to the pattern of the tear and the quality of the remaining ACL tissue. Unfortunately, only about 10% or less of patients had this type of tear off the femur bone, now commonly referred to as a Sherman type 1 or Sherman 1 bundle type 1 tear. These patients who have had successful ACL repair have generally had faster and less painful recoveries than those undergoing reconstruction. This intuitively makes sense since only a portion of the native ligament has to heal instead of the entire ligament having to be replaced with cells from the patient, a process called ligamentization, that occurs with grafts.
The attraction of the BEAR implant in my practice is that it could expand the number of candidates for ACL repair or preservation to include Sherman type 2 tears. These tears still have much of the tissue on the tibia stump, and often have good tissue quality, but would not quite reach the wall of the femurif they were simply repaired with suture. Type 2 proximal tears are defined as tears within 75% - 90% of the way between the tibia to the femur. The BEAR implant may be able to bridge these small gaps in the tendon and allow the patients healing cells to reach the wall of the femur. In my practice, the BEAR implant is always added in conjunction with a primary repair of the native ligament. Currently, the standard practice is to perform reconstruction of type 2 tears.
It’s possible that the BEAR implant may eventually have the proven data to support its use in even type 3 or 4 tears – those where there is less stump remaining, and generally tissue quality is poor. At this time, I recommend reconstruction for these types of tears as the safest and most reliable option but will continue to follow the literature on this evolving technology as we look for its place among the options that we can offer patients with these injuries.

Photography courtesy of Dr. Tyler Williamson – Perfect Circles Photography – for more information or to purchase prints please visit – https://perfectcirclesphotography.com/








