
Going “Knee Deep”
The information provided below is intended as an educational resource intended for surgeons and trainees (medical students, postgraduate residents and fellows starting practice). The information included are my templates for patient expectations, handouts useful for counseling patients in the clinic, forms for completing letters and office paperwork, surgical operative note templates, and similar items. These are free to use for reference, but they should be edited as needed to suit your practice settings and should always be applied with clinical judgement to the treatment of individual patients. They are intended as guidelines and resources and do not constitute medical advice. Unintentional errors, intentional misuse, or unintentional misinterpretation or failure to update this information is the responsibility of the learner/user. Please reach out to me with specific questions.
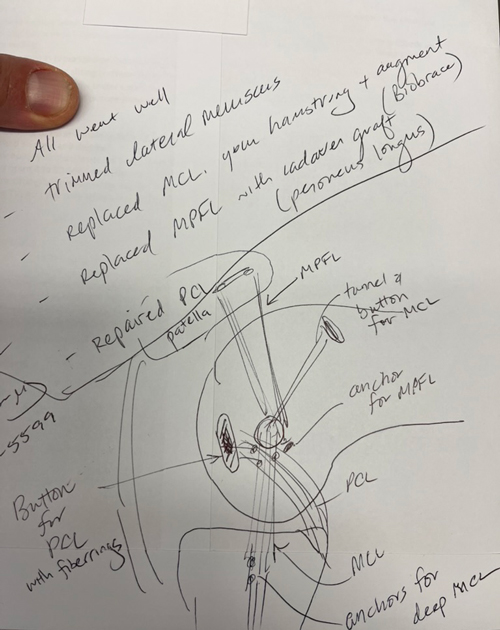
I myself am always learning and am far from perfect. As seen above in the photograph taken 10 years into clinical practice, I am always seeking to learn and better understand my own techniques and principles. Any adopted modified or evolving techniques will be updated here occasionally, but should not be taken at face value as the exact technique which I am currently using or use in any particular case as I modify each note and resource to suit specific circumstances, the same as I would in clinical care. Please use your judgement but I hope the following information is helpful.
Operative Note Templates
- ACL Auto Template
- ACL Quad Auto Template
- Ex Fix Knee Template
- ACL Repair Template
- ACL Allo Template
- Hardware Removal Template
- Knee MPFL and TTO Template
- OATS allograft Knee Scope Template
- Knee Scope Template
- OATS Knee Scope Template
- ORIF Tibial Plateau Fx Template
- Op Note - Generic
- PCL Allo Template
- Quad Tendon Repair Template
- Tibial Plateau ORIF Template
Surgery Case Preference Cards
- ACL Hamstring Autograft
- Arthroscopy-Distal Femoral Osteotomy with OATS
- ACL Recon ALLOGRAFT
- Arthroscopy-Biocartilage
- ACL Repair vs Recon ALLOGRAFT
- Arthroscopy-Oats
- Meniscus Repair
- MPFL Recon with Allograft
- Meniscus Root Repair
- Arthroscopy
- PCL All Inside- Allograft
- PLC Posterolateral Corner Reconstruction PLC
- PCL
- ACL Recon QUAD AUTOGRAFT
- ACL Repair vs Recon QUAD AUTOGRAFT
- Knee-MCL,LCL Repair
Knee Deep Blog
Visualizing Complex Multiligament Knee Reconstruction
Dr. Chip Routt once taught me that if you can draw it you can understand it and be a better surgeon. While my drawings are not up to the same level as Dr. Routt, I do like to sketch procedures for my patients, especially the more complex ones, like this example of a PCL primary repair with Arthrex FiberRings and repair tightrope, MCL reconstruction with Conmed Biobrace augmentation and an MPFL reconstruction. I generally like to repair more of these severe medial capsular injuries but this one presented closer to 3-4 weeks and we were not able to do as much with the native MCL and medial retinaculum as I would have liked. In severe injuries, particularly a femoral avulsion of the PCL, repair can be very gratifying, and if it fails can be converted to a reconstruction at a second stage. In most all multiligament cases, I stage the ACL reconstruction, do a planned lysis of adhesions and manipulation, reassess all meniscal and cartilage repairs, and check all the prior repairs or reconstructions. In some cases, the patient does not always need to return for that ACL reconstruction, but we talk about a second procedure at the 6 week postoperative visit. I have found that preparing patients for this earlier is helpful and less defeating than an ‘unplanned’ manipulation. The principle I like is: only one surgery that limits weight bearing and motion, and only limit it for 4 weeks. Certainly, no one has the perfect answer for these difficult cases, but I have found this approach to be utilitarian for many (but not all) situations.
Bone Grafting in Two-Stage ACL Revision
Two-stage ACL revision is sometimes unavoidable when prior tunnels are malpositioned, widened, or biologically compromised. I had a recent question:
How do you like to graft ACL tunnels?
In my practice, most revision tunnels aren’t neat cylinders—they’re irregular caverns. This is probably because I tend to see more soft-tissue grafts for revisions rather than BTB. And to be very honest, because I have to revise my own, too, and those tend to be all soft tissue. Because of this geometry, I’ve gravitated away from dowels and toward a chips + putty construct that can conform to the true shape of the defect.
Tunnel Preparation
I use a FlipCutter 3 on the femoral side, progressively enlarging and scraping the tunnel walls until I’m down to clean, bleeding bone. The process naturally creates a conical cavity rather than a uniform cylinder, which reinforces the need for a moldable graft. I tell our fellows you can run the flipcutter and use it like a “toothbrush” along the walls of the tunnel.
On the tibial side, I’ll typically ream to a 10 mm diameter at the joint line. Then this creates enough space for a camera and a currette up the tunnel from inferior. I’m careful to preserve the tibial aperture to avoid blowout into the anterior horns or tibial plateau. Visualization up the tunnel with the camera allows thorough debridement until only bone remains but I don’t typically have the trajectory exact and so again the currette will make an irregular shape but is selective about taking a minimum of bone and all of the old graft.
Graft Composition & Technique
My standard construct is:
- Cancellous chips + DBM putty, roughly a 1.5:1 ratio
- Mixed with a small amount of whole blood for handling and biologic enhancement
The goal consistency is simple: *think chocolate chip cookie dough* - packable, cohesive, and not soupy.
In cases where an anterior closing wedge osteotomy is performed, I’ll incorporate autologous tibial bone into the mix. In larger defects, this can approach a 1:1 ratio with allograft, autograft, with additional putty and blood to optimize volume and texture.
The photo below is Arthrex cortical fibers 7.5 cc mixed with the Allosync Pure 15cc, 7cc whole blood, and 5cc autograft tibia from the closing wedge.
I like the idea of PRP, but am not a patient person, so we use whole blood.
Delivery & Packing
The graft is packed into a cut 3 cc syringe, delivered arthroscopically:
- Femoral tunnel filled first, visualized from the lateral portal
- Digital packing around the femoral corner until firm (usually 3–5 cc)
- Tibial tunnel filled from distal to proximal with finger occlusion at the aperture, gently pressurized as it’s packed
Postoperative Protocol
Even with large tunnel defects, patients are allowed immediate weight bearing. With meticulous preparation and stable graft packing, incorporation has been reliable.











