Derotational Distal Femoral Osteotomy (DFO) for Excessive Femoral Anteversion
Max Whooley MS2, Kayla Aikins, MS3, Brian Gilmer, MD
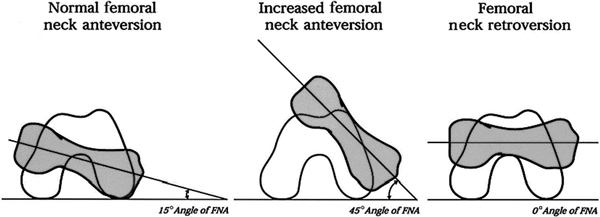
Derotational femoral osteotomy (DFO) is a surgical procedure performed to treat severe rotational abnormalities of the femur, such as femoral torsion. The femur is the longest bone in the skeleton and meets the pelvis to form the hip joint. Typically, femoral torsion ranges from 10-20 degrees anteversion1. Simply put, this is a measure of how much the femur bone is twisted between the hip and the knee joints. Normally, the hip points forward (anteriorly) about 17 degrees relative to the backs of the femoral condyles at the knee which are more or less close to parallel to the plane of the body. For genetic reasons, some patients have severe anteversion (knees pointing inward) or retroversion (knees pointing outwards opposite directions). When severe, the bone is sometimes cut to restore a more natural alignment of the femur. DFO is performed in children and adults who exhibit these abnormal alignments of the femur2.
It is worth noting that the position of the foot is not always indicative of the twist in the femur and patients do not always immediately notice this malalignment except that it causes pain at the hip or knee joint as they attempt to position the joint in abnormal positions in order to accommodate for the femoral rotation.
One common way this presents is with children who anatomically would prefer to intoe (so called ‘pigeon toed’) but gradually learn that this causes tripping over their own feet, or simply notice that other people do not walk this way. While the alignment itself is benign, pain can occur when children, often in adolescence start to correct this by positioning the foot forward. This causes an abnormal rotation at the knee because the joint is the only location where rotation can occur (since the bones cannot be moved by muscles but joint can). The patella, or knee cap, continues to attempt to travel directly in line as it is not attached except by a thin ligament to the rest of the femur. The end result is that the patella and femur do not align well and pressure builds under the knee cap particularly with activity.
In many cases, adolescents will gradually accommodate these changes and have some self-limiting pain which eventually resolves as they age. In some cases though, the pain becomes severe and debilitating preventing activity and even daily life without pain.
On top of this the abnormal alignment leads to an increased risk of the patella dislocating laterally. So while some patients only have pain, others have both pain and instability. In these cases, correcting the ligament alone (medial patellofemoral ligament reconstruction) is not enough to prevent the recurrent risk of dislocation again.
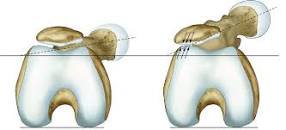
In this figure 1 there is increased pressure on the lateral side of the patella (lateral patellar facet compression syndrome) due to the femur being rotated more anteriorly (anteversion).
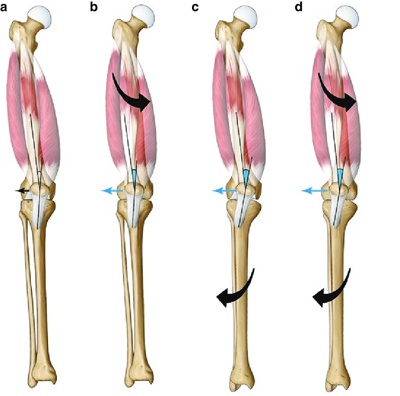
in this figure, the anteversion of the femur (second image from left) may be combined with external rotation of the tibial tubercle (third image from left) to cause a combined and complex ‘miserable malalignment’ (far right image). This is a controversial topic as some authors would argue that external rotation of the tibia tubercle is a radiographic rather than true anatomic phenomenon, but the important thing to understand is that anteversion can be combined with other problems such as trochlear dysplasia, external rotation of the tibial tubercle, or valgus (coronal plane alignment). We discuss these topics separately elsewhere in the encyclokneedia.
Indications
Derotational DFO is considered in Dr. Gilmer’s practice when anteversion is increased by at least 15 -20 degrees from the contralateral side (other leg) or both femurs are above what is commonly considered normal and the patient has symptoms that correlate to this malalignment. Normal ranges vary but are typically about 17-20 degrees. While there are no specific cutoffs, I will start to consider the procedure at around 35 degrees of anteversion or a difference compared to the other limb as above.
Causes
The exact cause of femur misalignment is not known, though genetic components and positioning in the womb may have contributions.
One question asked when evaluating persons with femoral anteversion is whether in childhood the patient sat as a ‘W’ rather than cross legged on the floor. When internal rotation from femoral anteversion is increased, external rotation is obligatorily decreased and so sitting in a cross legged position (criss – cross applesauce) will feel uncomfortable.
The above figure shows the characteristic “W” sitting of femoral anteversion
Diagnosis
Patients referred will generally have plain x-rays, a full length weight bearing alignment (52 inch xray) and a special CT scan which is called a CT anteversion protocol. This CT scan takes slices through the femur that can be compared to the knee and allows the surgeon and radiologist to calculate the amount of abnormal rotation.
If chondral or ligamentous pathology is suspected, an MRI can be performed3.
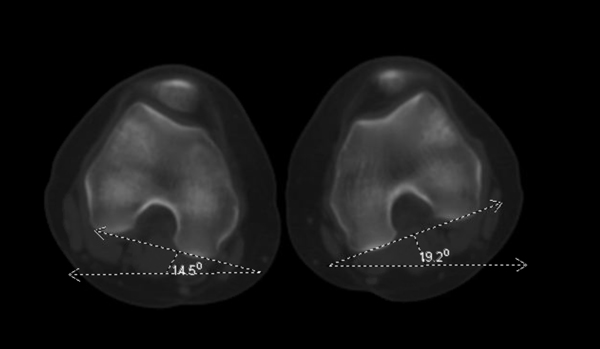 Figure 5
Figure 5
CT scanogram showing measurements of femoral anteversion
For completing this study, we generally provide a copy of the protocol instruction sheet as some imaging centers may be unfamiliar with obtaining this type of study, and, when performed properly, exposure to radiation can be substantially limited.
Procedure
The procedure for changing the alignment of the femur from side to side (coronal plane) which is done for varus (bow legged) or valgus (knock-kneed) deformities is also called a distal femoral osteotomy because in both cases the bone is cut (osteotomy) at the distal femur (part of femur bone just above the knee). Derotational osteotomy is done to untwist the bone so the cut is made in a different way.
Sometimes these deformities are combined and though it is possible theoretically to correct both deformities with one cut, this is beyond the ability of a surgeon and will most likely require further use of computer and robotic surgery in the future. It also tends to make the bone very unstable and at risk for non-healing or nonunion. All of this is to say, that typically only one or the other type of distal femoral osteotomy is performed except in some very rare and unique circumstances.
The procedure of distal femoral derotational osteotomy is often combined with other procedures such as knee arthroscopy or MPFL reconstruction to prevent the patella (knee cap) from dislocating again.
For the derotational DFO itself. An initial incision is made on the outside of the knee above the joint line. This incision is about the width of a hand based on the size of the patient. The iliotibial band is split and then a couple of metal wires are placed using a computer to determine the angle that will need to be corrected. For example, if the correction is 20 degrees, the pins are placed and measured so that they are 20 degrees relative to each other with one pin the top of the femur and one lower down by the knee.
The bone is then cut to allow the rotation to be corrected and the leg is spun until the wires become parallel. Then a metal plate is placed and secured with screws after being compressed together. No bone graft is needed.
 Figure 6
Figure 6
In this image, the wires have been placed in preparation for cutting the bone, the large pear shaped black object is a retractor placed to protect the major blood vessels and nerves behind the knee.
 Figure 7
Figure 7
In these images a metal plate and screws have been placed to hold the correction of rotation.The thin white line in the bone between the higher and lower screws is the location of the bone cut which has since healed.
Post-operative care
The procedure can be done as a same day surgery, or in some cases, an overnight stay is needed. Physical therapy starts immediately, within 3-5 days, and the knee can be bent to at least 90 degrees depending on what other procedures are performed. Ice should be applied during the first 2-3 days, and the patient should avoid all activities that propagate pain or swelling for at least a week. We usually let patients begin to bear some partial weight at 2 weeks and as they become more comfortable patients are free to bear weight and then they can start to walk normally. Full recovery can take 4-6 months.
We routinely check radiographs at 6 weeks and 3 months post-op to assess correction of the misalignment. Copies of the recovery protocol are available on the PT protocol page under patient information on the website.
Risks and complications
Risks of a rotational DFO include intra-articular fracture, neurovascular injury, knee stiffness, and overcorrection or under correction. These are in addition to the usual risks of surgery and anesthesia.
Dr. Gilmer’s Take
This is a powerful procedure which can really change a patient’s level of comfort and function in daily life and with activity. That being said, it is a major procedure that requires careful planning and execution. In my experience, patients in whom both legs are effected ultimately return to have the other leg corrected. I routinely plan for hardware removal in children and adolescents either 6 or 12 months after surgery typically during a summer or winter break from school. This second procedure has a much shorter recovery is done as outpatient surgery and has no immediate restrictions.
This procedure is rarely done in isolation and all other factors contributing either knee pain or instability or both should be evaluated to create a comprehensive approach. If you have questions about the procedure or would like a remote consultation please contact us
References
- Kulkarni RM, Ilyas Rushnaiwala FM, Kulkarni GS, Negandhi R, Kulkarni MG, Kulkarni SG. Correction of coronal plane deformities around the knee using a tension band plate in children younger than 10 years. Indian J Orthop. 2015 Mar-Apr;49(2):208-18. doi: 10.4103/0019-5413.152484. PMID: 26015611; PMCID: PMC4436488.
- Buly RL, Sosa BR, Poultsides LA, Caldwell E, Rozbruch SR. Femoral Derotation Osteotomy in Adults for Version Abnormalities. J Am Acad Orthop Surg. 2018 Oct 1;26(19):e416-e425. doi: 10.5435/JAAOS-D-17-00623. PMID: 30106763; PMCID: PMC6147096.
- Sabbag OD, Woodmass JM, Wu IT, Krych AJ, Stuart MJ. Medial Closing-Wedge Distal Femoral Osteotomy with Medial Patellofemoral Ligament Imbrication for Genu Valgum with Lateral Patellar Instability. Arthrosc Tech. 2017 Nov 6;6(6):e2085-e2091. doi: 10.1016/j.eats.2017.08.012. PMID: 29349001; PMCID: PMC5766318.
- Willey M, Wolf BR, Kocaglu B, Amendola A. Complications associated with realignment osteotomy of the knee performed simultaneously with additional reconstructive procedures. Iowa Orthop J. 2010;30:55-60. PMID: 21045972; PMCID: PMC2958271.
Kayla Aikins is currently a third-year medical student at the University of Nevada, Reno School of Medicine.
Max Whooley is a second-year medical student attending Creighton University School of Medicine in Phoenix, Arizona.