Osteochondral Autograft Transfer System (OATS) and Osteochondral Allograft Transplantation Surgery (OCA) with Precut Plugs
Victoria Maged, MS2
Introduction
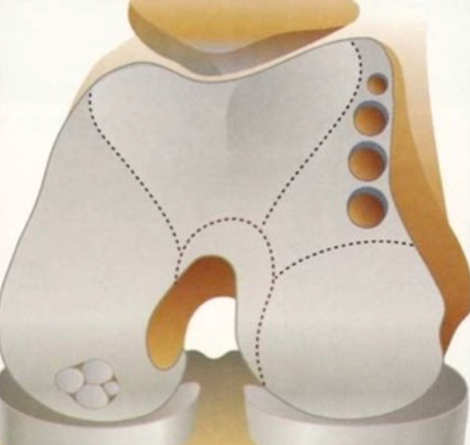
Joints are covered with articular cartilage that allows bones to move with little friction. Over time, wear and tear or injuries can degrade the cartilage, resulting is bones moving against one another and creating more injury and pain.1 An osteochondral autograft transfer system is a surgical procedure where healthy cartilage and bone from a non-weight bearing part of the patient’s knee is removed and implanted to the part of their knee that contains damaged cartilage.2 In an osteochondral allograft transplantation surgery, the healthy cartilage and bone comes from a donor rather than the patient, themselves, and is then transplanted into the area of damaged cartilage and bone in the patient.1 The goal of these surgeries is that the healthy cartilage and bone will start to grow into and heal the damaged area, providing the patient with symptom relief.2
Causes, Indications, and Contraindications
Patients who are candidates for an osteochondral allograft transplantation have large areas of damage ranging from 15 to 35 mm in diameter, symptoms of pain, swelling and catching, localized, full-thickness injuries, osteochondritis dissecans, avascular necrosis, previous failures of a surface chondral restoration procedure, degenerative arthritis, are younger than 50 years old, and are active with high physical demands.1,3,4,5 Patients who are candidates for an osteochondral autograft transfer system are also younger than 50 years old and can have the above symptoms and conditions, but they usually have minimal cartilage damage, typically less than 2 cm large, and plenty of healthy cartilage to use for the transfer.2 Typically, their cartilage damage resulted from a traumatic knee injury.2,3 Athletes are also affected by cartilage damage due to the high physical strain they undergo and related sports injuries, so they can be candidates for these surgeries as well.3,5
Contraindications include obesity, body mass index > 35 kg/m2, current tobacco use, active infection, bone cancer, osteonecrosis, generalized osteoarthritis, bipolar osteochondral lesions of the tibia and femur, ligamentous instability, alcohol abuse, inflammatory arthropathies, prolonged steroid use for a concomitant condition, uncorrectable mechanical alignment, abnormal patellar tracking, and meniscal deficiency.3,5,6,7
Diagnostics
Physical Exam
The physician will perform a knee exam to evaluate tenderness to palpation, passive and active motion, strength, ligament stability, lower extremity alignment, and gait.3 Knee swelling, quadriceps inhibition, and restricted passive and active motion can signal an intra-articular problem.3 Tenderness to palpation at or above the joint can point to a meniscal injury or chondral lesion of the femoral condyle.3 Patellar apprehension, patellofemoral crepitus, or a positive patellar grind test can suggest a patellofemoral defect.3 Atrophy of the quadriceps muscles may suggest a chronic injury.3 In addition, preoperative functional testing to obtain a patient’s baseline of functioning such as the Vail Sport Test can be done and includes single leg squats, lateral bounding, and forward and backward jogging.3 A Wilson’s test can also be done by internally rotating the patient’s foot and having them extend their leg while they are sitting down on the exam table.8 If they have knee pain that occurs 30 degrees from full extension and then disappears when their foot is externally rotated, they have a positive test for osteochondritis dissecans.8
Imaging
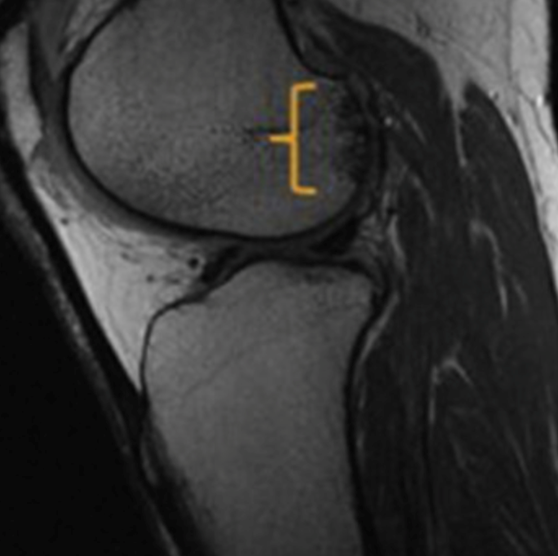
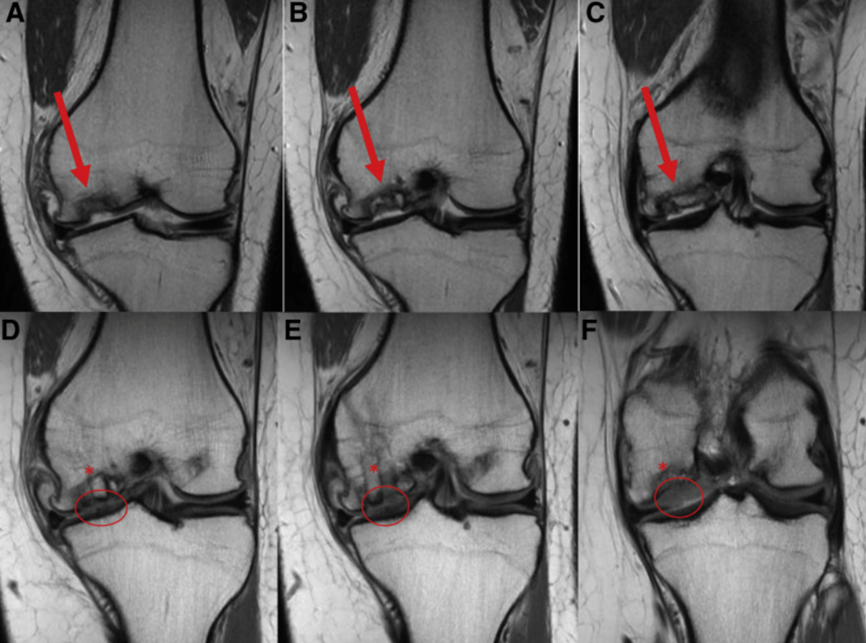
Radiographic knee evaluation includes bilateral weight bearing anteroposterior, lateral, 45-degree flexion posteroanterior, and patellofemoral views to evaluate for any bone abnormalities.3,6 Sizing markers help match the allograft’s size to the size of the damaged area of bone and cartilage.3 Standing long axis views of the lower extremities can be used to evaluate the mechanical axis as well as if surgery is warranted and if the graft may be predisposed to failing if genu varum or valgum malalignment is seen.3 Knee MRIs can be done to evaluate articular cartilage defects and help with measuring the size of a lesion if present.3 They can also evaluate for ligamentous or meniscal injury and identify any subchondral edema.3,6 Lastly, CT arthrography can be used on patients who are unable to get an MRI done or have had previous failed cartilage repairs, allowing changes in the subchondral bone to be viewed.3
Procedure
OCA
General or spinal anesthesia will be used on the patient, and arthroscopy may be done.1,3 The surgeon will create an incision to visualize the damaged joint.1 The size of the bone and cartilage damage is measured and removed.1 A graft of healthy cartilage and bone is taken from a donor and prepared for transplantation which includes sterilization, testing for risk of disease transfer, and resizing to fit the damaged area.1 It is then pressed into the place where the patient’s damaged bone and cartilage was removed and is secured with screws and pins if necessary.1,3 This surgery can be done through a variety of approaches depending on the location of the lesion as well as its shape and size. These include a dowel technique, shell technique, anterior approach, and posterior approach.4,7
OATS
General anesthesia is used on the patient, and the surgery will start with an arthroscopic examination of the knee.2,9 From there, the surgeon makes an incision on the knee and uses a coring tool to excise the damaged cartilage and bone.2 Then, the surgeon excises a piece of healthy cartilage and bone from a non-weight bearing part of the patient’s knee and places it into the area where the damaged bone and cartilage was previously removed.2,9
Postoperative Care
OCA
After surgery, a hinged knee brace locked in extension is worn for about 2 weeks.1,4 Patients are also prescribed medications for their pain.1,7 Patients can use crutches and limit weightbearing for 6-8 weeks until graft incorporation can be seen radiographically.1,7 Physical therapy starts early usually after the first postoperative visit and continues for 8-12 weeks.1,4 Range of motion increases from 0-90 degrees in the brace and then to full motion after 6 weeks.4 From there, gait training starts and progresses to full and unrestricted walking without crushes or a brace by 8-10 weeks.4 Resistance and impact are slowly increased at 18 weeks.4Full return to activity can occur anywhere from 6 months to a year after the surgery.1,4,7 Athletes can also start an advanced rehabilitation program after 3-4 months with a sports physical therapist but excessive loading on the allograft needs to be avoided.7
OATS
Pain medication will be prescribed after surgery, and a hinged knee brace will be used by the patient.5,6 Weightbearing is limited for 8 weeks.6 To help increase range of motion during the first 6 weeks, patients can use a continuous passive range of motion device as well as starting early on physical therapy to increase their range of motion from 0-90 degrees and then 90-120 degrees.5,6 From 6-12 weeks, full range of motion, a normal gait, and full proximal muscle strength is slowly regained.5,6 From 12-20 weeks, further strengthening exercises as well as agility exercises begin, so patellar mobility, stair climbing, progressive jogging, and plyometrics are focused on.5,6 After 20 weeks, sport related activities can be resumed, and full return to activity usually occurs 5-8 months after surgery.5,6
Risks and Complications
Some risks and complications include infection, knee swelling, pain, bleeding, graft failure, joint stiffness, blood clots, deep vein thrombosis, skin numbness around the incision, injury to vessels and nerves, and chronic pain syndrome.1,2,7
Dr. Gilmer’s Take
I prefer osteochondral autograft (OATS) for most cartilage and bone lesions in the knee which are small and on the condyles. In some cases, I will use them on the patella. In some cases, especially on the condyles, I prefer OATS for cartilage only lesions even when the bone seems ok. This is mostly because the recovery is faster than for MACI or other surface treatments and weightbearing can be started sooner because the OATS is immediately stable.
The advantages are that many lesions can be treated on the spot in a single surgery, whereas many other procedures require a second surgery (MACI, for example) and it can be done using the patient’s own tissue, which may integrate and heal better and be more durable. I have had excellent clinical results and thus it’s my preference to use OATS whenever possible.
The limitations of OATS are that there is only so much cartilage to take from. I have unfortunately had a couple cases of donor site morbidity, which is another way of saying pain from where the cartilage was harvested. In these cases, you can obtain allograft plugs OCA and fill the holes that the donor cartilage was harvested from. This has worked well but requires a second surgery and it has been difficult to get insurance companies to agree to what seems like the ideal case to me – transfer the autograft into the defect and then use allograft at the donor site at the first surgery. I have had colleagues who have had good success with this approach.
This OCA is different from the OCA where a whole condyle is used and so that is discussed elsewhere in the encycloKNEEdia under the OCA section. More information can be found there as it applies to larger lesions that involve bone and cartilage.
Brian Gilmer, MD
October 2023
References
- Frank, R.M. Osteochondral Allograft Transplantation. https://www.rachelfrankmd.com/osteochondral-allograft-transplantation-orthopaedic-surgeon-sports-medicine-specialist-denver-co.html
- Frank, R.M. OATS. https://www.rachelfrankmd.com/oats-orthopaedic-surgeon-sports-medicine-specialist-denver-co.html
- Haber, D.B., Logan, C.A., Murphy, C.P., Sanchez, A., LaPrade, R.F., & Provencher, M.T. (2019). OSTEOCHONDRAL ALLOGRAFT TRANSPLANTATION for the KNEE: POST-OPERATIVE REHABILITATION. International Journal of Sports Physical Therapy, 14(3), 487–499. https://doi.org/10.26603/ijspt20190487
- Anderson, Z.N., Lang, S.D., Haus, A., & Gilmer, B.B. (2022). Osteochondral Allograft Transplantation Of Posterior Femoral Condyle Lesions Utilizing An Open Posterior Approach To The Knee. Arthroscopy Techniques (Amsterdam), 11(8), e1487–e1492. https://doi.org/10.1016/j.eats.2022.03.040
- Vellios, E.E., Jones, K.J., & Williams, R.J. (2021). Osteochondral Autograft Transfer for Focal Cartilage Lesions of the Knee With Donor-Site Back-Fill Using Precut Osteochondral Allograft Plugs and Micronized Extracellular Cartilage Augmentation. Arthroscopy Techniques (Amsterdam), 10(1), e181–e192. https://doi.org/10.1016/j.eats.2020.09.025
- Guzman, A.J., Dela Rueda, T., Rayos Del Sol, S.M., Bryant, S.A., Jenkins, S., Gardner, B., McGahan, P.J., & Chen, J.L. (2021). Arthroscopic Osteochondral Autograft Transfer System Procedure of the Lateral Femoral Condyle with Donor-Site Backfill Using Osteochondral Allograft Plug. Arthroscopy Techniques (Amsterdam), 10(12), e2683–e2689. https://doi.org/10.1016/j.eats.2021.08.012
- Valdivia Zúñiga, C.A., & De Cicco, F.L. Osteochondral Allograft. [Updated 2022 Aug 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560511/
- Physiopedia. (2023). Wilson’s Test. https://www.physio-pedia.com/Wilson%27s_Test
- Raj, B.M. (2013 October 10). Overview of the OATS Procedure from a Los Angeles Orthopedic Surgeon. https://drhipandknee.com/overview-of-the-oats-procedure-from-a-los-angeles-orthopedic-surgeon/
Bio: Victoria Maged matriculated to the University of Nevada, Reno School of Medicine in 2021 and is currently a second-year medical student.








