Victoria Maged, MS2, Brian Gilmer, MD
Introduction and Anatomy
Patella alta is a type of patellofemoral dysfunction where the patella is superiorly displaced in relation to the femur, trochlear groove, or tibia.1,2 It can predispose patients to recurrent subluxation of the patella which leads to patellofemoral instability.2
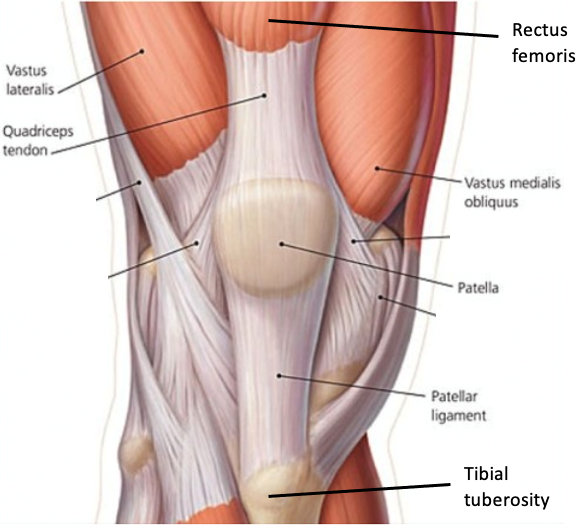
The patella is an upside down, triangle shaped, sesamoid bone anterior to the knee joint, which consists of the femur, tibia, and fibula. The patella sits over an area of the femur covered in articular cartilage3,4 The patellofemoral joint, specifically, is the space of the knee joint that lies between the patella and trochlea of the femur, which is the articular cartilage covered groove between the femoral condyles.3,4 Superiorly, it is connected to the quadriceps tendon, which is made up of the rectus femoris, vastus lateralis, vastus medialis, and vastus intermedius muscles.3,4 Inferiorly, the patella is connected to the patellar tendon, which inserts on the tibial tuberosity.3,4 When the quadricep muscles contract, they pull on these tendons with the patella to extend the leg.3

Presentation
History
Patella alta can commonly be found among patients with chondromalacia on the patella’s articular surface, patellar osteoarthritis, Sinding-Larsen-Johansson disease, Osgood-Schlatter disease, patellar tendinopathy, gait instability, recurrent subluxation of the patella, and anterior knee pain that worsens with activities such as running, jumping, and squatting.1,4,7,8 It can also be found among athletes, especially if they undergo a trauma or injury to the knee joint and/or related tendons.9
Physical exam
Patients with a unilateral patella alta may have a “nobbly knee” when they lay down and bend their knee 90 degrees.9 In this position, the patella will sit on top of the knee and tilt laterally.9
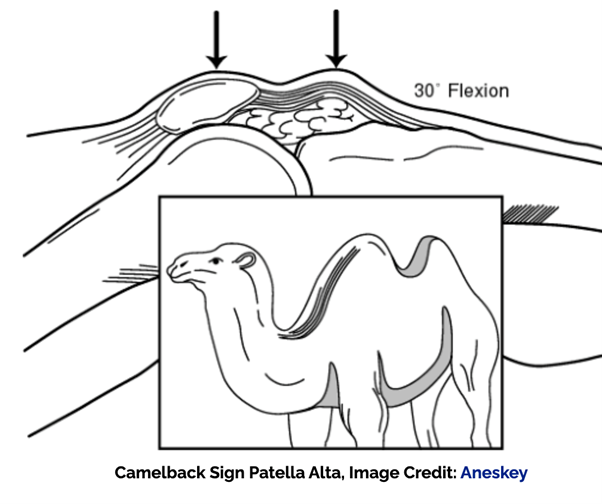
A camelback sign can also be present where two prominences are seen.8 One is due to the patella pointing upwards because of its position in patella alta, and the other is due to the natural presence of the tibial tuberosity.7,8
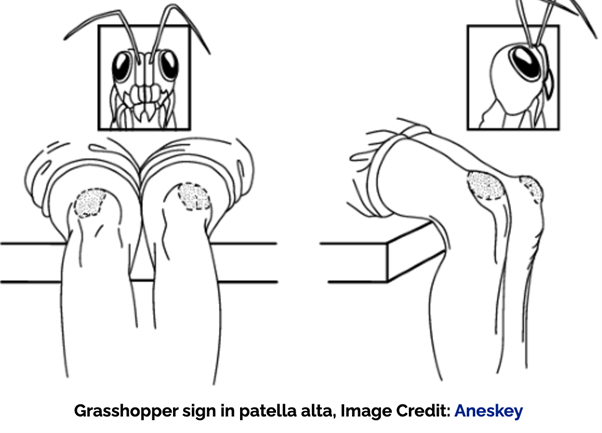
In addition, a grasshopper eyes sign can be present in those with bilateral patella alta.8 Here, both patellas sit high on each knee and tilt laterally, looking like the eyes of a grasshopper.8
A Fairbanks patellar apprehension test can also be done to evaluate for lateral patellar instability.7,10 When positive, the patient may pull their leg away from the physician and/or signs such as pain and muscle defensive contraction of a lateral patellar dislocation with 20-30 degrees of knee flexion can be present.10
A Patellar glide test can further evaluate for lateral/medial instability.10 It is positive when there is lateral/medial displacement of the patella greater than or equal to 3 quadrants.10
Imaging
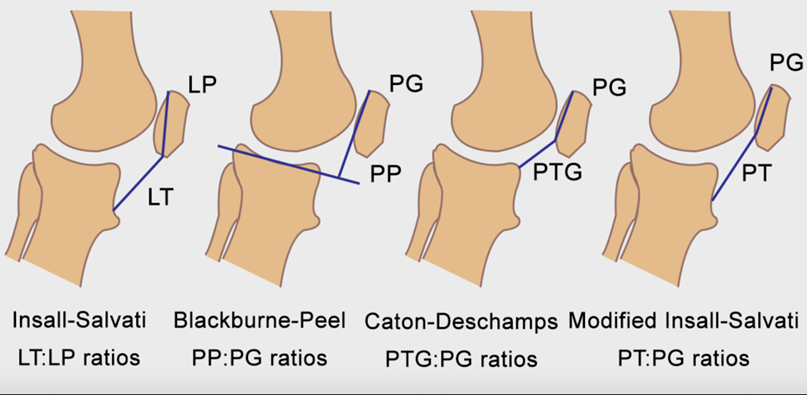
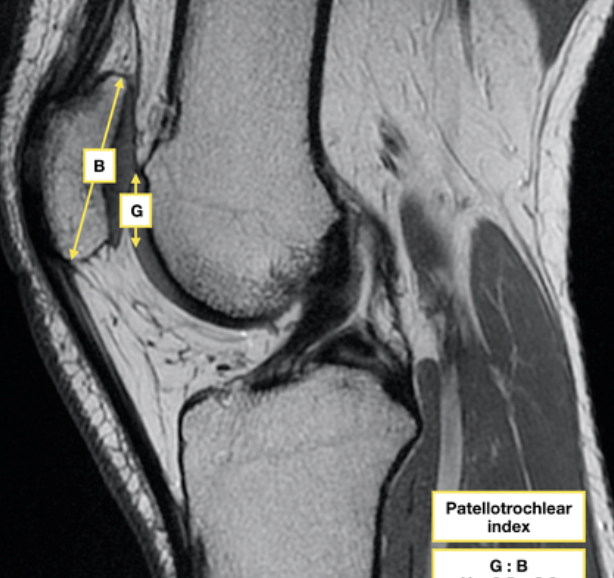
Four measurement methods can be used for diagnosis: lateral radiographs, radiograph ratios measured on MRI, patellotrochlear index (PTI) on sagittal MRI, and patellar tendon length measurement.2 Patella alta measurements include a Caton-Deschamps index >1.2, Insall-Salvati index >1.3, Blackburne-Peel index >1.0, PTI <0.125–0.28, and patellar tendon length>52 mm.2

Treatment
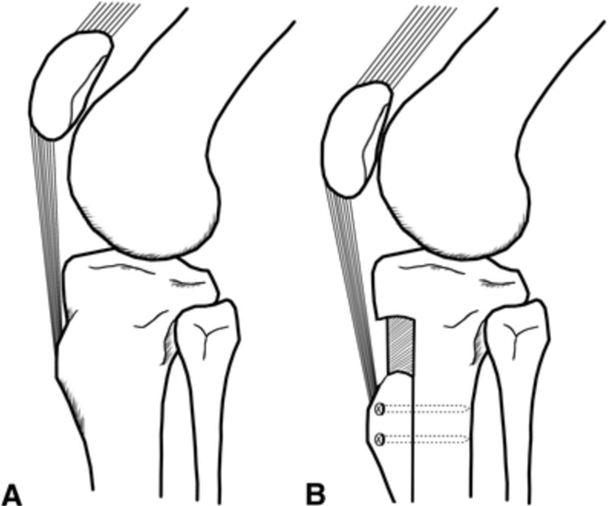
Initial treatment can include physical therapy, taping of the knee, and using a soft brace to help improve patellar stability and strength.2 When these treatments no longer provide relief and symptoms worsen, surgical procedures can be used to correct patella alta. In distalizing tibial tubercle osteotomy, the tibial tuberosity with the attached patellar tendon is moved distally so the patella moves inferiorly back into the correct position, and then, the tibial tuberosity is held in place with screws.2 Patients eligible for this procedure include those with recurrent patellar dislocations, patellofemoral pain, Hoffa impingement, and patella alta cartilage lesions.2
Another procedure called patellar tendon imbrication can be done for patella alta and lateral patellar instability in skeletally immature patients such as children and teenagers.15 Soft tissue procedures like these are done to prevent injury to and premature closure of the proximal tibial physis.2 During the procedure, multiple sutures are threaded into the patellar tendon, shortening its length and bringing the patella down into its correct position. 2
Dr. Gilmer’s Take
I generally consider adding treatment of patella alta when the overlap between the patella and the trochlea is close to 0 and a patient’s patella can be manually manipulated and is clearly still above the groove with the knee in 10 -20 degrees of flexion. I will reassess this at various levels of flexion to see where the patella enters the groove. I prefer this to any of the measurements as they can be somewhat inconsistent and the symptoms and exam seem better aligned with what the patient perceives.
If a tibial tubercle osteotomy (TTO) is already planned to move the patella centrally I will add distalization by a calculated amount to reduce patella alta.
In cases where a tubercle osteotomy may be contraindicated, either because the patient had one previously or because the growth plate on the tibia is still open, I will perform a patellar tendon imbrication.
There is some evidence that MPFL reconstruction alone will reduce patella alta and additional concerns about patellar compression which can cause pain or cartilage wear with distalizing and the risk of stiffness are all factors are all taken into account when considering when, how, and to what degree correcting patella alta should be done.
This is rarely done in isolation and is typically combined with MPFL reconstruction and possible other procedures as noted above.
Brian Gilmer, MD
October 2023
References
- 1. Holtzman, G.W., & Harris-Hayes, M. (2012). Treatment of patella alta with taping, exercise, mobilization, and functional activity modification: A case report. Physiotherapy Theory and Practice, 28(1), 71–83. https://doi.org/10.3109/09593985.2011.566910
- 2. Biedert, R.M. (2022). Patella Alta. Clinics in Sports Medicine, 41(1), 65–76. https://doi.org/10.1016/j.csm.2021.07.002
- 3. Cox, C.F., Sinkler, M.A., & Hubbard, J.B. Anatomy, Bony Pelvis and Lower Limb, Knee Patella. [Updated 2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519534/
- 4. Netter, FH. 2006. Atlas of Human Anatomy (4th ed.). Saunders Elsevier.
- 5. The Orthopedic & Sports Medicine Institute in Fort Worth. (2023). Knee Anatomy. https://www.osmifw.com/orthopedic-diseases-disorders/knee-injuries-disorders/knee-anatomy/
- 6. Rogers, C. (2022, May 11). ACL Injuries. https://hughston.com/wellness/acl-injuries/
- 7. Al-Sayyad, M.J., & Cameron J.C. (2002). Functional outcome after tibial tubercle transfer for the painful patella alta. Clinical Orthopaedics and Related Research, 396(396), 152–162. https://doi.org/10.1097/00003086-200203000-00024
- 8. Singh, A.P. Patella Alta Causes, Presentation and Treatment.https://boneandspine.com/patella-alta/#clinical-features
- 9. London Sports Orthopaedics Clinic. (2023). Patella Alta - High Riding Patella.https://sportsortho.co.uk/treatment/patella-alta-high-riding-patella/
- 10. Physiopedia. (2023). Patella Alta. https://www.physio-pedia.com/Patella_alta
- 11. Weerakkody, Y., Knipe, H., Niknejad, M., et al. (2011 February 23 ) Patella Alta. https://doi.org/10.53347/rID-13055. https://radiopaedia.org/articles/patella-alta?lang=us
- 12. General Health. Everything You Need to Know About Patella Alta. https://healthhearty.com/everything-you-need-to-know-about-patella-alta
- 13. Chmiel-Nowak, M., & Knipe, H. (2020, June 4). Patellotrochlear Index. https://doi.org/10.53347/rID-78481. https://radiopaedia.org/articles/patellotrochlear-index?lang=us
- 14. Yin, Liao, T.-C., Yang, L., & Powers, C. M. (2016). Does Patella Tendon Tenodesis Improve Tibial Tubercle Distalization in Treating Patella Alta? A Computational Study. Clinical Orthopaedics and Related Research, 474(11), 2451–2461. https://doi.org/10.1007/s11999-016-5027-5
- 15. Hinkley, P., Fletcher, C., & Strickland, S. (2022). Patellar Tendon Imbrication for the Treatment of Patella Alta in Skeletally Immature Patients. Arthroscopy Techniques (Amsterdam), 11(9), e1577–e1582. https://doi.org/10.1016/j.eats.2022.05.002
Victoria Maged matriculated to the University of Nevada, Reno School of Medicine in 2021 and is currently a second-year medical student.








