Patellar Instability - Dysplasia and Trochleoplasty
Sawyer Bauer MS3, Brian Gilmer, MD
Anatomy and Biomechanics of the Knee
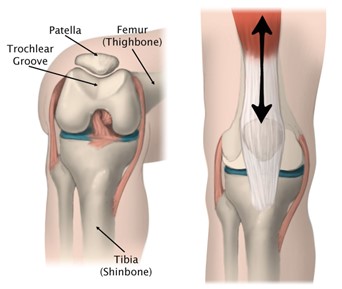
The patella is the largest sesamoid bone in the body serving to centralize and transmit extension forces from the four quadriceps muscles around the tibiofemoral joint and to the patellar tendon. This additionally serves to protect the tibiofemoral joint by providing a bony shield at the anterior surface of the joint, particularly on flexion when the joint is further exposed [1]. The patella is connected at its superior surface to the quadriceps tendon, and on its inferior surface to the patellar tendon. The posterior surface of the patella is divided into two surfaces, the superior (articular) surface and the inferior (non-articular) surface [2]. The articular surface lies in the trochlear groove (also called the femoral sulcus) of the distal femur, which maintains appropriate tracking during tibiofemoral joint flexion [1]. The trochlear groove deepens moving distally, deviates laterally from the axis of the femoral shaft and ultimately joins the articular surface between the lateral and medial femoral condyles. The femoral angle measures the depth of the trochlear groove and typically presents at 138±6° [1]. This central groove is lined by the medial and lateral facets which serve as a barrier to prevent pathologic medial or lateral movement of the patella in the anatomically normal knee. The knee engages these surfaces in different amounts throughout the flexion-extension cycle as the forces change [1].
Trochlear Dysplasia
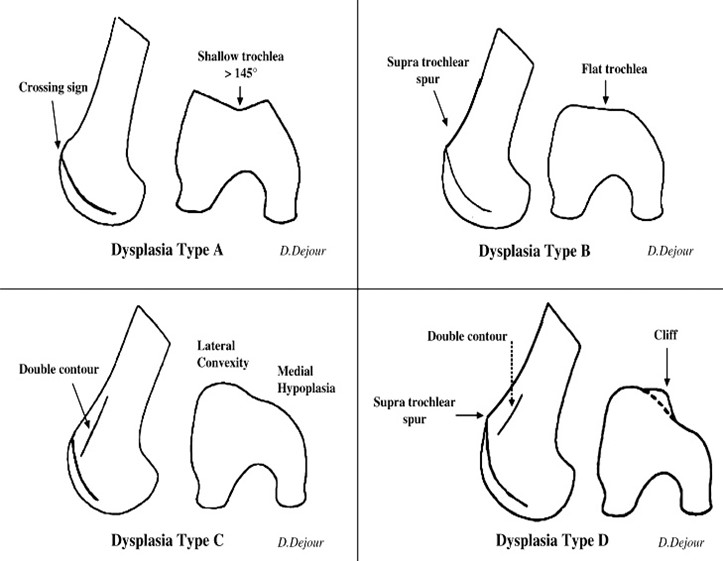
The biomechanical function of the patellofemoral joint relies heavily on the trochlear groove anatomy, therefore alteration in this anatomy may influence joint stability and function, potentially resulting in patellar instability. Patellar instability is any condition where the patella may pathologically disarticulate from the patellofemoral joint [3]. Trochlear dysplasia represents a particular type of patellar instability due to bony change or variation in the trochlear groove, medial, or lateral facets [4]. A defining feature of trochlear dysplasia is flattening of the trochlear groove, where the sulcus angle is increased 145 degrees or greater and defined as a shallow trochlea [4]. This decrease in depth results in instability and may present as pathologic lateral displacement of the patella [4]. Anatomic alteration of the trochlear groove and decreased resistance to lateral patellar translation places increased stress on the medial soft tissue restraints, particularly the medial patellofemoral ligament (MPFL) [4].
Patient History
Patellar dislocation is estimated at 5.8 cases per 100,000 individuals but is increased in the primary at risk population (those 10 to 17 years of age) to 29 cases per 100,000 individuals [4]. Recurrence in individuals is often very high with conservative treatments (15% to 44%) and the chance of a third dislocation following a second increases to 50% [4]. This high probability of recurrence often makes treatment a necessity due to the lack of spontaneous remission. A detailed patient history is important to discern between acute dislocation and chronic instability, as chronic instability may confer additional future damage to the joint. Patient’s may describe a “giving way”, “popping out’, or ‘dislocating’ sensation. In addition, the patient will often feel pain, will have a limited range of motion and may describe weakness in knee extension.
Physical exam
Inspection may reveal a laterally and/or proximally (patella alta) deviated patella relative to the trochlea, as well as bruising, swelling or effusion due to damage of the joint lining and muscles. The clinician should check for patellar mobility and excessive laxity. To test for lateral mobility the clinician can divide the patella into quarters from medial to lateral, and when lateral directional force is applied the normal patella should remain within 2 quadrants compared to the resting state [4]. Additionally, the patellar apprehension test may be used to assess patellar laxity. The patellar apprehension test is done by applying lateral force on the patella as the knee transitions from full extension into flexion, which may mimic a lateral patellar dislocation [5]. A positive test is defined as visible apprehension or activation of the quadriceps muscles. A ‘J” sign is indicative of patellar dislocation and is observed when the patellar tendon pull is not in line with the trochlear groove.

Imaging
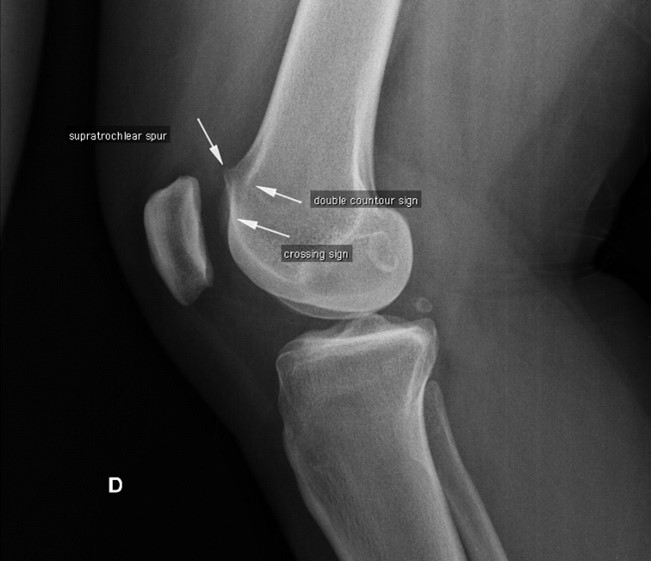
Interobserver reliability of physical examination when assessing patellofemoral joint instability is relatively poor and therefore along with a history and comprehensive physical exam, trochlear dysplasia is best evaluated using an objective assessment such as imaging [6,7]. A true lateral plain film radiograph may demonstrate the “crossover sign”, as well as supratrochlear spur and double contour, which in conjunction can assist in classification according to the Dejour Type [8]. In addition, this radiographic imaging may show signs of other pathologic states contributing to malalignment, such as a fracture. It is important true lateral x-rays are accomplished, as minor rotation may result in underestimation of dysplasia signs [6]. Further imaging with CT or MRI is mandatory to confirm grading of trochlear dysplasia [6]. Particularly, trochlear dysplasia is most often identified on MRI with abnormal trochlear height of the medial trochlear facet, which was seen in 83% of patients in one study. Further, 17% of patients exhibited an abnormal isolated lateral trochlear height, providing less lateral restraint of the patella [6].
Trochleoplasty
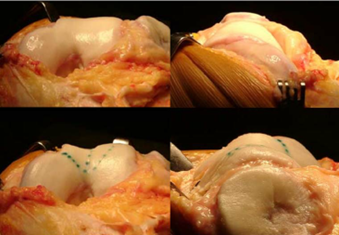
Patients with recurrent lateral patellar dislocation, and particularly with types B and D (High Grade) trochlear dysplasia are surgically indicated for correction via trochleoplasty [6]. Trochleoplasty consists of removing subchondral cancellous bone underneath the trochlear groove, with an aim of deepening the sulcus angle and having a new trochlear groove aligned flush with the anterior femoral cortex [6]. Trochleoplasty requires an incision over the patella to expose and open the lateral capsule, and medial retraction of the patella. The periosteum and trochlear cartilage are detached from the subchondral bone to create a flap, which is replaced after subchondral remodeling of the trochlear groove. If indicated, reconstruction of other tissues, such as the MPFL, may be performed. Rates of patellar dislocation recurrence following trochleoplasty are estimated to be low, with one systematic review reporting 2.4%, demonstrating it to be an effective treatment and significantly improve patient quality of life [10,11]. Patients with signs of patellofemoral arthritis, trochlear cartilage wear, skeletally immature patients and isolated patellofemoral pain without true episodes of patellar dislocation are contraindicated in trochleoplasty. Further, patients with types A and C trochlear dysplasia are not good indications for surgical correction via trochleoplasty [9]
Post-operatively patients can immediately bear weight with crutches and an extension knee brace. Rehabilitation consists of quadriceps and hamstring strengthening. Patients are free to run at 12 weeks and may return to sports starting at 6 months [9]. Individual patient clearance and assessment is required to maximize surgical treatment success. Individualized approaches should focus on appropriate surgical intervention and should treat any soft tissue or cartilage injury resulting from patellar instability.
Dr. Gilmer’s Take
Trochleoplasty is a surgical procedure that is used to treat recurrent dislocation or subluxation of the patella, or kneecap. This condition is often caused by trochlear dysplasia, which is a developmental anomaly of the knee joint (von Knoch, M., Böhm, T., Bürgi, M. L., von Knoch, F., & Bereiter, H., 2006).
Trochleoplasty aims to reshape the trochlear groove in the femur, where the patella fits, to prevent the patella from dislocating (von Knoch, M., Böhm, T., Bürgi, M. L., von Knoch, F., & Bereiter, H., 2006).
There are several techniques for trochleoplasty, including the Bereiter technique, the Dejour technique, and the Goutallier technique, each of which has its own advantages and disadvantages (von Knoch, M., Böhm, T., Bürgi, M. L., von Knoch, F., & Bereiter, H., 2006).
Although trochleoplasty is a complex procedure, it has been shown to significantly improve knee function and reduce pain in patients with trochlear dysplasia (Thélu, C.É., Frank, F., Gagey, O., & Marteau, E., 2016). References: 1. von Knoch, M., Böhm, T., Bürgi, M. L., von Knoch, F., & Bereiter, H. (2006). Trochleaplasty for recurrent patellar dislocation in association with trochlear dysplasia. A 4- to 14-year follow-up study. The Journal of Bone and Joint Surgery. British volume, 88(10), 1331–1335. https://doi.org/10.1302/0301-620x.88b10.17875 2. Thélu, C.É., Frank, F., Gagey, O., & Marteau, E. (2016).
Trochleoplasty procedures show complication and reoperation rates similar to other patellofemoral surgeries. Knee Surgery, Sports Traumatology, Arthroscopy, 24(10), 3176–3183. https://doi.org/10.1007/s00167-015-3588-9
I attended residency with a colleague who traveled to Europe and learned the procedures from its orginators there. When he returned, I learned the technique, and while it remains uncommon in the United States, it has been a tremendously powerful tool for what has historically been a very difficult problem.
Patients with dysplasia have a much higher incidence of patellar dislocation because the groove in which the patella rides is quite shallow.
The groove deepening procedure allows for correction of alignment in the coronal plane (side to side) as well as deepens the groove, and can offload the cartilage when there is wear from maltracking. This is always performed with an MPFL reconstruction and lateral lengthening to adjust the soft tissue tension of the joint.
Many of these patients have had prior surgery and because of the shallow groove have had recurrent instability and failed prior ligament reconstruction alone. In some cases I will perform this as the first surgery, but more commonly it is after prior failed surgery.
I use a stepwise approach to look at the factors that are known to contribute to patellar instability: patella alta, dysplasia, MPFL insufficiency, lateral tracking, and patellar tilt as well as assessing the growth plates, overall limb alignment (typically valgus) and cartilage condition as well as the patient’s age and goals. I call this approach the ‘patellofemoral worksheet’ and it allows me to create an approach that addresses all of the patient’s risk factors as needed
My most common indication for trochleoplasty is a Dejour B trochlea and a lateral trochlear incliniation angle less than 10 (normal is 20), and I use a Bereiter technique that lifts the cartilage as a flap then fix it with absorbable suture and anchors.
Brian Gilmer, MD
Last updated: October 2023
Citations
- Tecklenburg K, Dejour D, Hoser C, Fink C. Bony and cartilaginous anatomy of the patellofemoral joint. Knee Surg Sports Traumatol Arthrosc. 2006;14(3):235-240. doi:10.1007/s00167-005-0683-0
- Al-Imam A, Al-Zamili Z, Omar R. Surface Area of Patellar Facets: Inferential Statistics in the Iraqi Population. Anat Res Int. 2017;2017:2685159. doi:10.1155/2017/2685159
- https://orthoinfo.aaos.org/en/diseases--conditions/patellofemoral-arthritis/
- Wolfe S, Varacallo M, Thomas JD, Carroll JJ, Kahwaji CI. Patellar Instability. In: StatPearls. Treasure Island (FL): StatPearls Publishing; September 18, 2022.
- Ahmad C.S., McCarthy M., Gomez J.A., et. al.: The moving patellar apprehension test for lateral patellar instability. Am J Sports Med 2009; 37: pp. 791-796.
- LaPrade RF, Cram TR, James EW, Rasmussen MT. Trochlear dysplasia and the role of trochleoplasty. Clin Sports Med. 2014;33(3):531-545. doi:10.1016/j.csm.2014.03.005
- Smith TO, Clark A, Neda S, et al. The intra- and inter-observer reliability of the physical examination methods used to assess patients with patellofemoral joint instability. Knee. 2012;19(4):404-410. doi:10.1016/j.knee.2011.06.002
- Kazley JM, Banerjee S. Classifications in Brief: The Dejour Classification of Trochlear Dysplasia. Clin Orthop Relat Res. 2019;477(10):2380-2386. doi:10.1097/CORR.0000000000000886
- Hinckel BB, Arendt EA, Ntagiopoulous PG, Dejour D. 2015. Trochleoplasty: historical overview and Dejour technique. Oper Tech Sports Med. 23(2): 114-122.
- Leclerc JT, Dartus J, Labreuche J, et al. Complications and outcomes of trochleoplasty for patellofemoral instability: A systematic review and meta-analysis of 1000 trochleoplasties. Orthop Traumatol Surg Res. 2021;107(7):103035. doi:10.1016/j.otsr.2021.103035
- Orfanos G, William Glover A, Sharma N, Barnett A. Trochleoplasty for severe trochlear dysplasia significantly improves the quality of life of patients with symptomatic patellar instability. Knee. 2022;37:95-102. doi:10.1016/j.knee.2022.06.003
- Dejour D, Saggin P. The sulcus deepening trochleoplasty-the Lyon's procedure. Int Orthop. 2010;34(2):311-316. doi:10.1007/s00264-009-0933-8
Sawyer Bauer
Sawyer Bauer is a second-year medical student from the University of Nevada, Reno School of Medicine with an interest in orthopedic surgery and musculoskeletal injury.









