
Unicompartmental Knee Arthroplasty (UKA) Surgeon in Reno, NV
Unicompartmental knee arthroplasty (UKA) is a joint-replacing surgery for patients with unicompartmental knee osteoarthritis that causes instability, swelling, pain, and deformity. Dr. Gilmer provides diagnosis and individualized non-operative and operative treatment plans in Reno, NV. Dr. Gilmer also provides highly specialized care during and after the surgery. Contact Dr. Gilmer’s office for an appointment today!
Sahar Forootan Sedigh, MS2 and Brian Gilmer, MD
Overview
Unicompartmental knee arthroplasty (UKA) is a joint-replacing surgery for patients with unicompartmental knee osteoarthritis that causes instability, swelling, pain, and deformity. 1 of the 3 compartments of the knee joint (Fig. 1), either the medial tibiofemoral (most common), lateral tibiofemoral, or patellofemoral, are replaced in UKA. Severe arthritis of the knee can be debilitating; therefore, UKA allows for enhanced mobilization, faster recovery, and improved function with minimal complications. It has a shorter surgical duration and is a less invasive procedure.
There are 3 major knee joint compartments:
- Medial compartment (most common)- Articulation between the medial femoral condyle and medial aspect of the tibial plateau
- Lateral compartment - Articulation between the lateral femoral condyle and lateral aspect of the tibial plateau
- Patellofemoral - Articulation between the patella and the femoral trochlear groove

Figure 1. A description of the cartilage that protect the bones of the knee. These compartments are damaged due to wear and tear, leading to UKA for pain management and functional improvement.
Image retrieved from: www.orthoinfo.aaos.org
Alignment of the knee is an essential component of load distribution, with any shifts in the neutral alignment leading to osteoarthritis. Varus (bow-legged) malalignment leads to increased stress in the medial knee compartment, causing osteoarthritis (Fig. 2). Valgus (knock-kneed) malalignment causes osteoarthritis to occur in the lateral knee compartment. Those with malrotation and maltracking (patella moves sideways from its groove when the leg is bent or straightened) will present with patellofemoral osteoarthritis.
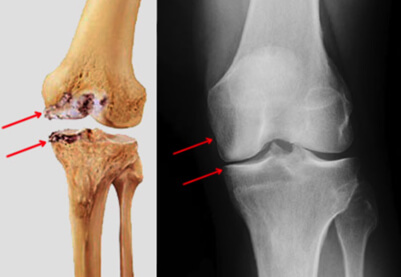
Figure 2. Red arrows indicate medial compartment osteoarthritis.
Image retrieved from: www.hss.edu
Indications
UKA is recommended for patients that have significant arthritis in one compartment, especially those that are younger with a mild to moderate osteoarthritis. Patients should have a BMI < 40, have intact knee ligaments, and no knee alignment issues. Age, range of motion of the knee, bone structure, and exercise frequency all help determine if the patient is a candidate for UKA.
Medial UKA
- Steady joint with intact cruciate ligaments
- Lateral compartment is in good condition
- Flexion contracture of <10 degrees
- Varus malalignment that is minor in damage
Lateral UKA
- Steady joint with intact cruciate ligaments
- Medial compartment is in good condition
- Valgus malalignment that is minor in damage
Patellofemoral UKA
- Debilitating pain and impairment that occurs during daily activities
- Middle-aged patient
- Non-inflammatory patellofemoral osteoarthritis
- Patellofemoral dysplasia without malalignment
Symptoms
- Knee pain that is exacerbated with activity
- Decreased range of motion in knee
Diagnosis
Diagnosis includes a thorough physical exam performed by the orthopaedic surgeon to determine if the patient is a good candidate for UKA. X-ray and MRI are used to assess the location and size of the knee compartment damage.
Procedure
An epidural, regional anesthesia, or femoral nerve blocking agent will be used as an anesthetic. The surgeon will begin with a small incision near the site of the affected compartment. A 3-5in incision is made above the damaged compartment in front of the knee. Structures in the area such as the ligaments and patella will be moved aside to assess the damaged area, which will be removed with some underlying bone to allow for the implants to be cemented into place. CT-guided imaging may be used to aid in the procedure.
UKA is the removal of the arthritic cartilage with replacement using a specialized metal (titanium, chrome/cobalt alloys, zirconium alloys) that attaches to a synthetic polyethylene plastic (Fig. 3 and 4). This minimizes the wear for abrasion that would normally occur. For medial or lateral compartments, the implant will be cemented to the bone. For patellofemoral UKA, the patellofemoral cartilage is removed and replaced with a polyethylene that will articulate with a metal femoral component. After testing for proper range of motion and function of the joint, the tissue will be sutured. Surgery will take anywhere between 1-2 hours.

Figure 3. A metal plate topped with a synthetic bearing that can be either fixed or mobile. In this example, the implant is attached in the medial knee compartment.
Image retrieved from www.understand.com
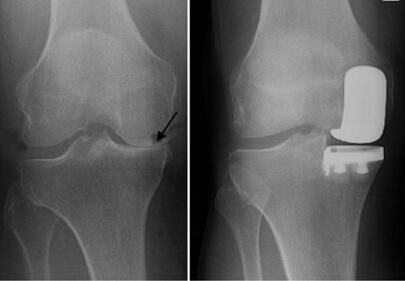
Figure 4. Osteoarthritis is seen in the medial compartment (arrow) followed by a successful UKA.
Image retrieved from: orthoinfo.aaos.org
Post Op
UKA is a less invasive surgery so patients will have a quicker recovery time. The surgeon may prescribe opioids (reviewed per patient history) or recommend NSAIDs for pain management. The patient will need to begin weightbearing exercises immediately after surgery. A walker or crutches may be recommended for several days or weeks. Follow up visits will be required with the orthopaedic surgeon.
Risks and Complications
Patients that have inflammatory arthritis, crystal arthropathy, severe patellar maltracking, and tibiofemoral arthritis may be ineligible for UKA. It’s important to monitor for DVT, signs of infections, and lack of full knee extension by 4-6 weeks.
One of the risks of a UKA is the potential need for revision to total knee arthroplasty (TKA). This is most commonly due to osteoarthritis developing in another knee joint compartment. Other more rare reasons include infection, unsolved pain, instability, polyethylene bearing dislocation (Fig. 5), or aseptic loosening of the femoral component1. Surgical revisions can consist of adding another UKA, changing UKA to total knee arthroplasty (TKA), or revising one UKA to another.

Figure 5. A and B show a 3-mm dislocated bearing which is replaced with an 8-mm think bearing(C) and a reduction in the valgus angle (D).
Dr. Gilmer’s Take
With careful selection, patients can be very happy with partial knee replacement or UKA because of the more natural feeling of the joint, the preservation of all the ligaments, and the faster recovery compared to total knee replacement. It is critical to ensure that the pain is limited to one compartment, usually the medial or inside of the knee, and I will sometime order an MRI to evaluate the cartilage in other parts of the knee. In other cases, I will assess the space on the rest of the knee with stress xrays to test the cartilage in another part of the knee.
Currently, I prefer the medacta Moto implant for medial and lateral UKA and the Arthrex IBalance patellofemoral joint replacement for replacement under the knee cap area. More information about the Medacta implant is available here: patients.medacta.com
Note: As of the date of publication Dr. Gilmer has no financial relationship with Medacta as a company and prefers this implant because of its excellent clinical results in practice, ease of use, and familiarity. Excellent outcomes can be achieved with a variety of implants by different manufacturers.
References
- Ji, J. H., Park, S. E., Song, I. S., Kang, H., Ha, J. Y., & Jeong, J. J. (2014). Complications of medial unicompartmental knee arthroplasty. Clinics in Orthopedic Surgery, 6(4), 365-372.
- Luo, T. D., & Hubbard, J. B. (2022). Arthroplasty Knee Unicompartmental. In StatPearls [Internet]. StatPearls Publishing.
- Murray, D. W., & Parkinson, R. W. (2018). Usage of unicompartmental knee arthroplasty. Bone Joint J, 100(4), 432-435.
- Sharma, L., Song, J., Felson, D. T., Cahue, S., Shamiyeh, E., & Dunlop, D. D. (2001). The role of knee alignment in disease progression and functional decline in knee osteoarthritis. Jama, 286(2), 188-195.
- Walker, T., Perkinson, B., & Mihalko, W. M. (2012). Patellofemoral arthroplasty: the other unicompartmental knee replacement. JBJS, 94(18), 1712-1720.
Sahar Forootan Sedigh, MS2
Sahar Forootan Sedigh is a second-year medical student at the University of Nevada, Reno School of Medicine.
Resources
Dr. Gilmer generally prefers the Medacta Moto medial unicompartmental knee for partial medial knee replacement which is the most common. He also prefers this system for the lateral compartment although the instrumentation is slightly different for the lateral side of the knee since the anatomy is also different.
More information about the Medacta MOTO Medial Knee Replacement can be found here Moto Medial Partial Knee
In some cases Dr. Gilmer may recommend the MAKO robotic assisted partial knee replacement. More information on this system is included below.
Unicompartmental Knee Replacement (UKR) Update 2025 – Patient Information
Preservation of the ACL and Proprioception
One of the key advantages of unicompartmental knee replacement is the preservation of the anterior cruciate ligament (ACL). Maintaining the ACL helps retain natural knee stability and enhances proprioception-the body’s ability to sense joint position and movement. This can lead to better coordination, balance, and a more natural feeling after surgery.
Implant Options and Customization
I prefer to use the Medacta MOTO medial and lateral knee implants for most unicompartmental procedures. These implants are designed to fit the knee’s anatomy precisely, providing excellent outcomes. In some cases, I may opt for the Kinemed Kinematch system, which is tailored to the patient’s uniqueanatomy based on detailed CT scans. This personalized approach is especially helpful when addressing knee dysplasia, as the patellofemoral joint can vary significantly from patient to patient. Customization helps ensure a better fit and reduces the risk of complications.
Use of Robotic Assistance
When indicated, I utilize robotic technology to enhance surgical precision. The choice of robotic platform depends on the facility: I typically use the Stryker or DePuy systems, both of which are highly advanced and reliable. Robotic assistance can improve implant positioning and overall outcomes.
Survivorship and Longevity Data
Unicompartmental knee replacements have demonstrated excellent durability. The failure rate is approximately 1% per year over 20 years, with some studies showing about 1.5% per year for medial and lateral compartments. The patellofemoral compartment tends to have a slightly higher failure rate of around 2% per year. Patients requiring patellofemoral replacements are often younger, but overall, many patients in their 50s or early 60s-rather than the 60s or 70s typical for total knee replacements-are good candidates, depending on their knee condition.
Patient Demographics and Age
Many unicompartmental patients are younger, often in their 50s, but there is a bimodal distribution. Some older patients, typically over 80, experience significant pain relief with less surgical risk and a quicker recovery. The decision is based more on the condition of the knee rather than age alone.
Preoperative Evaluation
Before surgery, I usually obtain an MRI to assess the cartilage condition in other parts of the knee. This helps identify potential issues like lateral patellofemoral tracking problems or wear, which could impact outcomes or necessitate revision. X-rays are also used as screening tools, and I generally avoid operating if there is significant wear (greater than grade 2) in the unaffected compartments. Most decisions regarding whether to perform a partial or total knee replacement are made well before surgery, rarely during the procedure itself.
Outcome Expectations
The success of unicompartmental knee replacement is influenced by surgeon experience and volume. While some surgeons prefer to perform only total knee replacements, I believe that the decision should be a shared process between myself and the patient, considering the specific knee condition and personal goals.
Recovery and Rehabilitation
For detailed information about expected recovery timelines and protocols, please visit the “Knee Deep” section of my website under “Recovery Protocols.”
If you would like to have additional information on the treatment of various knee conditions or would like to learn more about Unicompartmental Knee Arthroplasty (UKA), please contact Dr. Gilmer, serving the communities of Reno, NV.








