Cyclops Lesions
Joseph Gardner, MS-2, Brian Gilmer, MD
Introduction
Cyclops lesion is a complication that may occur following an anterior cruciate ligament reconstruction(ACLR). A cyclops lesion ,also known as localized anterior arthrofibrosis, is a fibrous nodule of granulation tissue located in the anterior region of the graft from ACLR. Cyclops lesions contribute to be cyclops syndrome only when the lesion impedes the extension of the knee. Of the 250,000 ACL reconstructions in the U.S. per year there is a 1-10% reported incidence of cyclops lesions. It is assumed that many lesions go unreported because they are asymptomatic and have no impediment to the healing process.1

Figure 1: Image of cyclops lesion on anterior cruciate ligament graft with knee in extension.

Figure 2: Image of cyclops lesion on anterior cruciate ligament graft with knee in flexion.
Risk Factors
Certain factors are known to have higher chances of the development of cyclops lesion:
- Female sex because of narrow notch1
- Increased volume of graft in relation to the notch size1
- Bony avulsion of anterior cruciate ligament (ACL) from tibia1
- Bony avulsion of ACL from femur1
- Anterior placement of tibial tunnel1
- Double-bundle ACL reconstruction because of higher volume of graft1
- Hamstring contracture1
Diagnosis
Most cyclops lesions are diagnosed within the first 6 months after ACLR. Patients will show symptoms of the inability to fully extend their knee and a have a positive bounce sign (patients knee ‘bounces’ back into flexion once full extension is reached). While sometimes unnecessary for the diagnosis, an MRI is often performed to confirm the presence of the cyclops lesion and plan for excision, or to assess for other pathology in the knee prior to surgery.
Notably, these patients will have failed to achieve extension from the beginning of recovery and this generally remains the case throughout the progression of rehabilitation. A cyclops lesion is often suspected at the 6 month visit and if it is persistently symptomatic is often treated shortly after the 3 month visit. That being said, treatment can be undertaken even later in the course of recovery with good success.
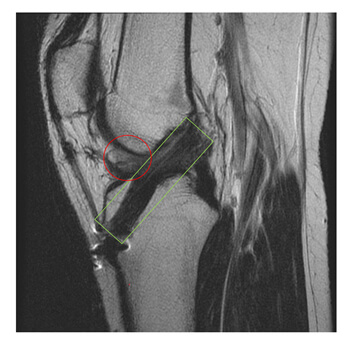
Figure 3: MRI of knee following an ACLR. The green box shows the anterior cruciate ligament graft. The red circle shows the cyclops lesion on the anterior aspect of the graft. Of note, the MRI image here corresponds to the same patient with the arthroscopic images seen above.
Treatments
When extension of the knee is compromised and cyclops syndrome is diagnosed a secondary arthroscopic debridement is performed by shaving the fibrous lesion away. It is generally not recommended to remove an asymptomatic cyclops lesion detected on an MRI that was obtained for other reasons.1
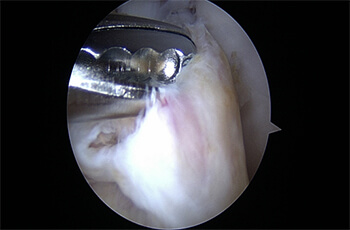
Figure 4: Image of the debridement of a cyclops lesion

Figure 5: Image of anterior cruciate ligament graft after the cyclops lesion has been removed.
Prevention
There are recommend strategies to follow to lower the likelihood of the development of cyclops lesion:
- Delaying ACLR until after recovery of ROM1
- Minimally invasive surgery compared with open ACLR1
- Creating less debris by use of a sequential reamer and thorough removal of debris1
- Correct tunnel positioning1
- Debridement in and around the bone tunnel1
- Notchplasty (reconstruction of intercondylar notch to avoid impingement of the graft2) if associated with impingement of the ACL graft1
- If possible, drawing the graft from the femoral tunnel first into the tibial tunnel to draw debris into the tibial tunnel1
- Early postoperative mobilization1
Even when these strategies are employed, cyclopshas been noted to develop in some patients without apparent underlying risk factors.
Dr. Gilmer’s Take
Cyclops lesions may be more common after ACLR with quadriceps tendon autograft because the graft has a larger volume than bone tendon bone or hamstring grafts (BTB or HS, for more information please see related section on ACL reconstruction and graft choices.
I try to mitigate this risk by harvesting a smaller graft that is better suited to patient size and geometry of the intercondylar notch that accomodated the native ACL. This frequently means harvesting an approximately 10mm graft in larger males and 9mm graft in smaller females or adolescents.
In my practice which contains a high volume of ACL patients, cyclops lesion is quite rare – approximately one case per year among over 100 ACL reconstructions annually. Fortunately, the treatment is straightforward and often lends itself to a minimally invasive approach with a needle arthroscope or nanoscope. Typically patients may initiate immediate weightbearing and resume their standard postoperative course without ultimate delay in return to sport or activity.
I do receive a handful of referrals per year for patients with chronic cyclops lesions and have had good success with simple excision and a focused rehabilitation program that emphasizes regaining terminal extension. For a remote consultation please contact us.
References
- 1) Kambhampati SBS, Gollamudi S, Shanmugasundaram S, Josyula VVS. Cyclops Lesions of the Knee: A Narrative Review of the Literature. Orthopaedic Journal of Sports Medicine. 2020;8(8). doi: 10.1177/2325967120945671
- 2) Kitridis D, Tsifountoudis I, Georgiannos D, Tsikopoulos K, Givissis P, Bisbinas I. Does Bone Regrow After Notchplasty in ACL Reconstruction? A Prospective Computed Tomography Study With 2-Year Follow-up. Orthopaedic Journal of Sports Medicine. 2021;9(9). doi:10.1177/23259671211029228
Joseph Gardner is a second year medical student at the University of Nevada, Reno and is assistant editor of the EncycloKNEEdia online library.








